Medicare Supplement Insurance
Avoid paying what Medicare Parts A & B don't cover! Whether you are new to Medicare or seeking a different Medicare Supplement plan, we simplify the Medicare Supplement Insurance process and get you the lowest rates possible.
Understand Your Medicare Supplement Options
Get the Lowest Rates Available for Medicare Supplement Insurance
Rates can vary greatly between Insurers. The least expensive policy one year may not be the next. Be sure to shop your plan annually on the month before your birthday. In California, a Medicare Supplement insured has the right to change to the same plan level or lower without answering health history or underwriting questions. For example, you can move from Company A’s active Plan F to Company B’s Plan F if you apply 30 days before or after your birthday. This is what the insurance industry calls a Guarantee Issue under the “California Birthday Rule.”
It is also important to compare rates from as many carriers as possible. If you purchased your policy directly with a carrier and they say you are paying the lowest rate possible, you’re not really shopping your policy. That insurer will only tell you the best rates they have – not the best rates available on the open market. Look beyond an agent that only represents one or two carriers. It is best to contact an insurance broker that represents multiple insurance carriers and plans.
Contact Margy Wenham Insurance Services when shopping Medicare Supplement. She represents most major insurance carriers doing business in California and can get you the lowest rate.
What is a Medicare Supplement Plan?
Medicare Supplement Insurance, also known as a Medigap Plan, is sold by private insurance carriers and helps fill "gaps" in Original Medicare. Original Medicare covers a large portion of the cost of health care services and supplies, but not all of them. That’s where the Medicare Supplement Plan comes in to help pay some of the remaining health care costs like copayments, coinsurance, and deductibles.
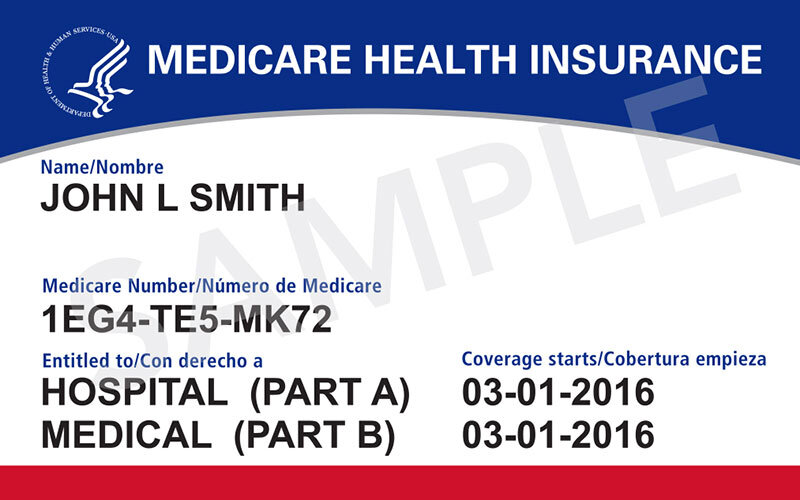
In order to purchase a Medicare supplement you must have Medicare Part A and Part B. You can sign up for Medicare at your local Social Security Office or on Social Security's website. A Medigap policy is different from a Medicare Advantage plan. An Adavantage plan covers most Medicare services, but they are not paid for under your original Medicare. A Medigap policy only supplements your original Medicare benefits Part A and B benefits.
Original Medicare
Medicare is a government health-care program that will pay for medical expenses such as doctor visits, hospitalization, and surgery.
The majority of people of the United States receive the right to participate in Medicare when they reach the age of 65. Eligibility is determined by whether you have worked the necessary number of hours and made the required payroll tax payments over the course of your life. People who do not meet the requirements may still enroll in Medicare, but will have to pay a higher premium.
Medicare is Divided Into Four Parts:
Part A: Hospitalization and Some Skilled Nursing
Part B: Out-of-Hospital Expenditures
Part C: Medicare Advantage Plans
Part D: Prescription Drug Plans
Most people who participate in Medicare Parts A and B will also buy a Medicare Supplement or Medicare Advantage Plan to help offset expenses that Medicare does not cover.
Helpful Resources
Medicare Supplement Plans
Medicare Parts A & B are required. Medicare Supplement Plans help to offset expenses that Medicare Parts A & B do not cover.
A Medicare Supplement Plan differs from a Medicare Advantage Plan. A Medicare Supplement Plan only supplements the Original Medicare benefits, while Advantage Plans are ways to get Medicare benefits.
Medicare Supplement Plans require a monthly fee. This monthly premium is in addition to the Medicare Part B premium you pay monthly to your private insurance provider.
Only one individual is covered by a Medicare Supplement Plan. You'll have to buy separate policies if you and your partner both want Medigap coverage.
A Medicare Supplement Plan can be purchased from any insurance provider. The insurance provider that the Medicare Supplement Plan is purchased from must be licensed to sell them in your state.
If you have health conditions, every standardized Medicare Supplement Plan is guaranteed renewable. This ensures that as long as you pay your premiums, your Medigap coverage will not be cancelled.
Prescription drugs are covered by certain Medigap plans sold in the past. However, prescription drug coverage is not allowed in Medicare Supplement Plans sold after January 1, 2006. You can join a Medicare Prescription Drug Plan (Part D) if you need prescription drug coverage. If you purchase both a Medicare Supplement Plan and a Medicare Drug Plan from the same provider, you may be required to pay two premiums. To find out how to pay your premiums, contact your provider.
If you have a Medicare Advantage Plan, it is illegal for someone to sell you a Medicare supplement plan. Unless, that is, you are switching back to Original Medicare.
Medicare Supplement Plan FAQs
How much does your service cost?
The service we provide to you is completely "free". When you apply for a Medicare Supplement Insurance policy, we get paid a fee directly from the insurance company for our service.
How do I enroll in basic Medicare Parts A & B?
You can apply online to enroll in Medicare Parts A & B here. Additionally, you can call the general Social Security local phone number at (866)964-1236.
What exactly is a Medicare Supplement (MediGap) Plan?
Medicare Supplement Insurance, also called MediGap, is a secondary form of insurance that people on Medicare will purchase to fill the coverage gaps present in Medicare. Medicare only covers a portion of healthcare expenses, and without a Medicare Supplement Insurance Plan, you will likely be left with hundreds, if not thousands of dollars in out-of-pocket expenses when you need healthcare.
Will I get a better price if I apply directly through the insurance company?
No. Medicare Supplement Prices are fixed by law. The insurance company charges the exact same price, regardless of how you purchase or sign up for a policy.
Will I receive ID cards for my new policy?
Yes. After you are approved for your new Medicare Supplement Policy, it generally takes about 1-2 weeks to receive your new policy ID cards in the mail.
Why should I sign up through an independent broker like you?
When you sign up for your Medicare Supplement Policy through an independent broker, like me, you will obtain far better customer service than you will receive anywhere else. This is because the over-whelming majority of the policies we service are Medicare Supplemental Insurance. We strive very hard to know all of the latest changes and updates that our clients should be aware of. We are also always available for immediate customer support should you ever experience any problems or have any questions regarding your policy.
Is there a bias towards certain insurance companies?
No. Since we are an independent broker, that means we work on your behalf, not the insurance companies. We represent most Medicare Supplement Companies and are not biased toward any specific one. Our goal is to search through all plans, and all companies in order to find you the best Medicare Supplement Plan for the best price available.
When should I apply for a Medicare Supplement Policy?
It depends on your specific situation, but we recommend applying for a new policy approximately 2-3 months before you would like coverage to start. You first have to complete an application for a new Medicare Supplement Policy, then it has to be submitted to the insurance company to go through underwriting. Depending on the time of year, this process usually takes a couple of weeks.
What is a "Guarantee Issue Period"?
A Guarantee Issue Period is a specific right to purchase Medicare Supplement Insurance without answering any health questions, and being "guaranteed coverage". To name a few instances, you might be entitled to a guarantee issue period; e.g., if you are retiring and losing group health insurance, your previous health insurance plan is being terminated, you move out of state or out of your plans service area, etc. These are only a few reasons you might qualify for "Guarantee Issue" such as your first enrollment in Medicare Part B or it is the month of your birthday.